Getting a referral
Coordinating care and treatment for you and your family.
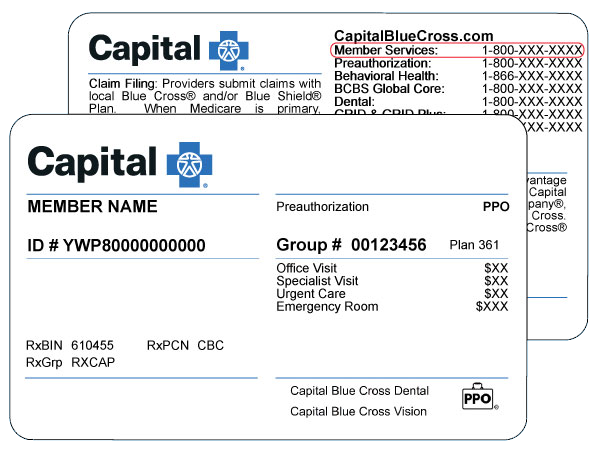
Do you have a health maintenance organization (HMO) plan or gatekeeper PPO plan? Check the suitcase on your member ID card.
If you have one of these benefit plans, your health care needs to be coordinated.
How does it work?
- Choose a primary care physician (PCP) for primary care (like checkups).
- Your PCP can refer you to other doctors and hospitals for specialty care (like surgery).
- Your care is covered by your benefit plan when you see your PCP or if your PCP referred you to a specialist in our network.
- If you get care from a doctor who is not in our network, the care would not be covered unless it is urgent or an emergency.
There are two types of referrals:
- Consult and treat: Your PCP sends you to a specialist who will decide what treatment you need. The specialist may send you to get more medical services (like diagnostic tests or outpatient surgery).
- Specified service: Your PCP sends you to a specialist for a treatment or service (like outpatient surgery).
Tips for making the most of your health care dollars:
- It is your PCP's responsibility to submit your referral documentation.
- You don't need referral documentation for claims that are less than $300.
- If you have an HMO: referrals are good for 90 days after the date of service (or at the end of your benefit plan year if that comes first).
- If you have a gatekeeper PPO: referrals are good for 360 days after the date of service (or at the end of your benefit plan year if that comes first).
- You don't need a referral for behavioral health care if the care is given by a provider in our network.
- You don't need a referral for obstetrician-gynecologist (OB/GYN) services if care is given by a provider in our network.