Population Health Management programs and services
Members can enjoy the benefits of our Population Health Management programs such as clinical care and health and wellness services.
We focus on the health and well-being of all our members
- Using advanced analytics, we customize programs to meet members where they are.
- Supports intervention strategies to optimize member health and promote healthier outcomes.
With a strategic focus on:
- Healthy: Keep the healthy, healthy
- Rising risk: Support individuals with early health conditions and intervene to prevent or delay progression of disease
- Chronic: Help people with chronic diseases; engage them in management of their disease to slow or stop its progression
- Catastrophic: Identify and manage the complex needs of the catastrophically injured and ill
Clinical care
Managed behavioral health
Behavioral health
For members with CHIP, group, or individual coverage1
Experiencing ups and downs in life is normal. However, when emotions or behaviors start to impact your health, family, or relationships, it’s time to find help.
We are here for you. We provide services to help manage concerns such as:
- Depression
- Autism spectrum disorder.
- Bipolar disorder.
- Generalized anxiety disorder.
- Substance use disorder.
Call 866.322.1657 to enroll.
Care/Disease management
Care/Disease management
For CHIP, group and individual product members
These services emphasize quality care and cost-effective health outcomes. These services are available to all eligible members. The program is based on Case Management Society of America (CMSA) and National Committee for Quality Assurance (NCQA) standards for all population health management, including program performance measures. Our program also uses disease-specific, evidence-based guidelines, and serves chronic and catastrophic populations by delivering quality care through interventions and collaboration with a focus on promoting health that prioritizes needs, actively coordinates care, and prevents readmissions.
Care managers work collaboratively with the member, his or her healthcare team, and his or her family to complete the case management process and develop a member-centric plan of care. They match identified needs with existing resources, including community-based and government-supported agencies and programs.
Members are eligible based upon claims, Providers can refer or members can self refer by calling 888.545.4512.
Care management
Asthma
For CHIP, group and individual product members
The major goals of the program are to help members improve their knowledge and self-management of asthma, and to help them effectively use available resources to treat the disease. The program has many areas of concentration; however, self-management, education, knowledge enhancement, and use of peak flow meter, action plan, and medication compliance are of particular importance.
Members are eligible based upon claims. Providers can refer or members can self refer by calling 888.545.4512.
Automated outbound calls
For CHIP, group and individual product members
Proactively addressing 4 areas of clinical care
- Low Risk Maternity: Follows member through pregnancy (tips/education). Confirms delivery/postpartum care
- Low Risk Condition Support (Adult/Ped): Support for those with certain disease states; COPD, asthma, congestive heart failure (CHF), coronary artery disease (CAD), low back pain, and diabetes
- Care Management Awareness (Adult/Pedi): Explain CM program and transfer to Care Manager
- ER Utilization – (Adult/Pedi): Confirm use of ER and identifies barriers
Members are eligible based upon claims. Providers can refer or members can self refer by calling 888.545.4512.
Coronary artery disease
For group and individual product members
The major goals of the program are to improve the participant’s quality of life. The program works to empower participants so they can self manage the disease with the help of a personalized plan. The program has many areas of concentration with self-management, education, appropriate use of medications, weight and fluid management, and referrals to a cardiologist being of particular importance.
Members are eligible based upon claims. Providers can refer or members can self refer by calling 888.545.4512.
Chronic obstructive pulmonary disease
For group members
The major goals of the program are to improve the participant’s quality of life. The program works to empower participants so they can self manage the disease with the help of a personalized plan. The program has many areas of concentration with self-management, education, appropriate use of medications, smoking cessation, and referrals to a pulmonologist being of particular importance.
Members are eligible based upon claims. Providers can refer or members can self refer by calling 888.545.4512.
Depression
For CHIP, group and individual product members
This program is designed to focus on symptom recognition and behavior modification. The Depression program only accepts participants who have been screened by an internal care management program. Adult and senior participants referred for Depression Management are screened internally and referred to the program if they are determined to be high-risk.
Pediatric participants are excluded from the internal program. Pediatric participants with depression who have been screened and referred by another care management program will be referred to the Behavioral Health management.
Members are eligible based upon claims. Providers can refer or members can self refer by calling 888.545.4512.
Diabetes
For CHIP, group and individual product members
The major goals of the program are to improve the participant’s quality of life. The program works to empower participants so they can self manage the disease with the help of a personalized plan. The program has many areas of concentration, with self-management, education, and glucose, lipid, and blood pressure control being of particular importance.
Members are eligible based upon claims. Providers can refer or members can self refer by calling 888.545.4512.
Heart failure
In conjunction with the at home remote monitoring program
For group and individual product members
Our goal is to improve the quality of life for our members with heart failure. The program empowers participants to self manage the disease with the help of a personalized plan that helps slow progression, avoid complications, and promote medication adherence and physician follow-up care. Our Care Managers work closely with members, their providers, and cardiologists to prevent emergency room visits and hospitalizations, and lower the readmission rates.
Members are eligible based upon claims. Providers can refer or members can self refer by calling 888.545.4512.
Low back pain
For group members2
The major goals of the program are to improve the participant’s quality of life. The program works to empower participants so they can self manage the condition with the help of a personalized plan. The program has many areas of concentration, with self-management, education, appropriate use of pain medications, weight management, and exercise being of particular importance.
Members are eligible based upon claims. Providers can refer or members can self refer by calling 888.545.4512.
Maternity management
For eligible group and individual product members5
Our maternity management program provides educational information, care coordination, and support to women who are expecting.
We focus on helping pregnant members:
- Find and engage a healthcare practitioner
- Receive recommended pregnancy and preventive care
- Make lifestyle changes
- Adhere to their practitioner’s treatment plan
- Engage with clinical and educational resources, as appropriate
- Reduce risk
- Increase maternity health literacy
Providers and members may call 888.545.4512 and request an eligibility determination..
High-risk maternity management
For group and individual product members5
Members identified as high-risk receive direct outreach from an assigned nurse, who has extensive experience in all phases of pregnancy and delivery, including high-risk labor and delivery, newborn care, and post-partum care. The nurse-based telephonic program is an opt-in program.
Providers and members may call 888.545.4512 and request an eligibility determination..
Women’s health and family support
For group and individual product members3,4
Your health plan may offer the enhanced version of Ovia Health, which includes two women’s health apps that provide support through life’s biggest transitions: planning or starting a family, navigating pregnancy and postpartum, balancing life as a busy parent, and managing menopause.
Qualified members receive unlimited support from a team of health coaches including registered nurses and certified nurse midwives, and get expert content, tips, and personalized health insights – including support for spouses or partners, too.
Download the Ovia Heath app that meets your needs.
Case management
Oncology
For CHIP, group and individual product members
Care Managers experienced in cancer care and advanced care planning provide assessment and support to members at all stages of a cancer diagnosis. This voluntary program offers members goal-oriented, individualized support through ongoing assessment, planning, and monitoring. Advocacy and linkage with other programs and community resources are key components of the program.
Members are eligible based upon claims. Providers can refer or members can self refer by calling 888.545.4512.
Transplant
For CHIP, group and individual product members
Care Managers experienced in transplant care provide assessment, education, and support during the transplant process. Core goals of this program include education and support regarding treatments, medical benefit plan, and locating Blue Distinction Centers for Transplants® 6.
Members are eligible based upon claims. Providers can refer or members can self refer by calling 888.545.4512.
Utilization management
Utilization management
For CHIP, group and individual product members
Evaluates the appropriateness, medical need, and efficiency of certain healthcare services, procedures, and facilities according to established criteria or guidelines, and under the provisions of the health plan benefits.
Applicable to all members for eligible services, procedures, facilities, etc.
Transition of care
For CHIP, group and individual product members
Focuses on the reduction of readmissions by ensuring that our members have everything needed to succeed at home upon leaving the hospital. A coordinator will contact eligible members within 24-48 hours of their discharge from acute care to ensure that all of their needs are met. The coordinator will make weekly calls to the member for 30 days.
Available to eligible members.
Other care management programs
Concierge services
For CHIP, group and individual product members
As part of our ongoing efforts to improve member health and strengthen member engagement, we help members with identifying “next best actions” they can take to actively engage in their healthcare and make beneficial changes.
For example, if a member with Type 2 diabetes calls our member services center and the representative notes the member has not had an A1C test in two years, the representative may remind the member of the test and help with getting an order form to the member’s doctor. The representative also can help locate the most convenient labs for the member to use.
Applicable to all members.
Managed second surgical opinion
For group members7
We can help eligible members seek expert medical services when they are facing complex and/or costly medical needs.
State-licensed doctors work directly with members, regardless of their geographic location, to provide them with:
- Expert second opinions
- Timely information relative to second opinion or diagnosis review
- Treatment plan advice
- Help navigating the virtual and in-person healthcare landscape
- Help finding the best in-network doctors near them
- Clinical support
- Mental health support
Check with your employer about the availability of this program.
Health and wellness programs
Healthy discounts program
For group and individual product members
With Blue365, members may receive fitness, nutrition, and other products and services at a discounted rate.
Visit Blue365Deals for more information.
Monthly member e-newsletter
For CHIP, group and individual product members
Members receive timely and relevant health plan information along with tips for better health and wellness
Members are automatically enrolled.
MyCare Finder
When members make smart healthcare choices, it can have a big impact on their bottom line.
Our new cost and care transparency platform offers best-in-class technology to help members easily find healthcare providers and compare the costs of healthcare services. MyCare Finder takes the guesswork out of finding in-network providers, hospitals, and services at the best price.
MyCare Finder delivers provider information, pricing, and recovery timelines for hundreds of medical conditions, allowing members to be more engaged as they navigate healthcare with greater confidence and control.
Visit our MyCare Finder page for more information.
Health promotion and wellness
Health and wellness programs
Preventive screening reminder program
For CHIP, group and individual product members
Our adult preventive health campaign uses social media, provider and member newsletter articles, and employer awareness to remind members about preventive screenings and encourage them to get these important services, which include immunizations, well visits, and cancer screenings.
For children, we send mailers and emails to parents of children who have preventive services included in their plan benefits. Through these campaigns, we encourage parents to schedule well visits for their children during which their healthcare provider can track their medical history, conduct physical and developmental assessments, and receive guidance about the needs of growing children.
Members are automatically enrolled.
Healthy Blue Rewards
For group and individual product members7
An engaging wellness platform that allows members to earn incentives for making informed decisions. The program offers a fun and reward way for members to participate in health and wellness activities that can help improve their health.
May be included with some individual plans.
Check with your employer about the availability of this program.
Online health assessment
For members with group and individual product
Taking a health assessment can help you learn about your strengths and areas where you can improve.
Your plan also includes free digital health tools that can help you find ways to be healthy and stay well. They include:
- Articles, quizzes, how-to guides, self-assessments, and recipes for healthy meals that can help you work healthy habits into your daily life.
- Content on health topics, including weight management, addiction, disease prevention, physical activity and safety, sleep habits, stress management, and emotional well-being.
Log in to your secure account to get started.
Online health content
For group and individual product members
Members have access to a free medical database through their secure member account. This resource provides a platform for members to become more active in their healthcare and encourages them to make smarter, more informed decisions. The content includes:
- Advice about making treatment decisions
- Information on health conditions
- Health and wellness topics
- Material on medical tests and medications
- Symptom checker
- Treatments for certain conditions and ailments
Log in to your secure account to enroll.
Diabetes prevention, management, and reversal programs
Digital diabetes programs for group and individual plan members7
One of these programs may be just what you need if you want to take control of your health goals, or if you’ve ever been told you have prediabetes or diabetes.
- Get personalized support from a professional health coach and diabetes specialists.
- Receive free supplies – You may get lancets, test strips, or a digital scale, based on the program and your specific needs.
- Get online community support and accountability.
- Lose weight and gain energy.
Learn more about the diabetes programs.
Empower
For group and individual product members
This program takes a health and wellness approach to help members create and maintain better lifestyle habits that support their weight management goals. Our virtual program is offered on-demand and features instructional videos and activities designed and delivered by health education experts who are also trained to help adults get the most out of a virtual learning experience.
Go to the Health and wellness coaching to enroll.
Take Charge
For group and individual product members
A Diabetes and Nutrition Program, Take Charge offers multiple sessions created and lead by a Registered Dietitian. With a focus on education and skill building, this program encourages lifestyle change through dietary modifications that help control blood sugars. Sessions include an overview of diabetes, nutrition and the food label, carbohydrate counting, meal planning, food preparation and measuring, and grocery shopping.
Go to the Health and wellness coaching to enroll
Capital Blue Cross Connect biometric screening
For CHIP, group and individual product members
Members can visit any Capital Blue Cross Connect health and wellness center to receive biometric (glucose, cholesterol, weight, etc.) screenings at no cost. Members also can get important health education information to keep them healthy and improve their biometric results.
Visit Capital Blue Cross Connect to enroll.
Capital Blue Cross Connect fitness classes
For CHIP, group and individual product members
Members can join free fitness classes covering several types of programs at all experience levels at our Health and Wellness centers.
Visit Capital Blue Cross Connect to enroll.
Capital Blue Cross Connect health coaching
For CHIP, group and individual product members
Health Coaching is provided by certified Well Coaches located at Capital Blue Cross Connect. The program covers a variety of topics such as nutrition, weight management, stress management, general motivational support, fitness.
Visit Capital Blue Cross Connect to enroll.
1Federal Employee Program (FEP) Members can learn more about their available programs or call 800.365.7986 for Behavioral Health Services.
2Available if a member’s employer includes with benefits.
3Ovia Health by Labcorp programs are available to eligible members ages of 18 to 64.
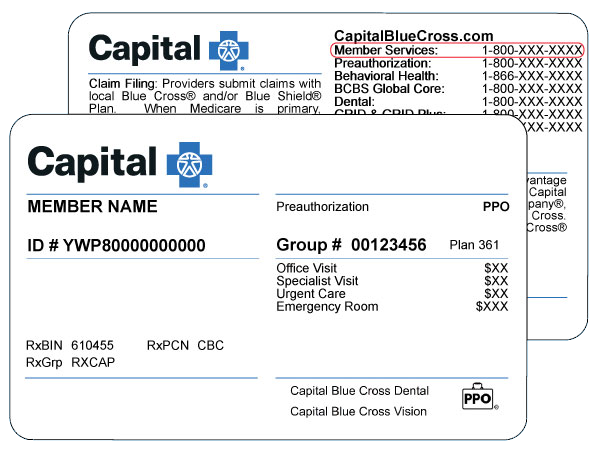
4Enhanced Ovia Health apps are offered at no cost to members under applicable plans. Call the number on your member ID card (TTY: 711) to confirm coverage.
5Our maternity management staff includes certified case managers, certified perinatal bereavement counselors, and lactation specialists.
6Blue Distinction Centers (BDC) met overall quality measures, developed with input from the medical community. A Local Blue Plan may require additional criteria for providers located in its own service area; for details, contact your Local Blue Plan. Blue Distinction Centers+ (BDC+) also met cost measures that address consumers’ need for affordable healthcare. Each provider’s cost of care is evaluated using data from its Local Blue Plan. Providers in CA, ID, NY, PA, and WA may lie in two Local Blue Plans’ areas, resulting in two evaluations for cost of care; and their own Local Blue Plans decide whether one or cost of care evaluation(s) must meet BDC+ national criteria. National criteria for BDC and BDC+ are displayed on the Blue Cross Blue Shield website. Individual outcomes may vary.
7These programs are covered at no cost to eligible members under most plans. Call the number on your member ID card (TTY: 711) to confirm coverage. If you receive health coverage through your employer, you can also contact your employer to confirm eligibility.
All information provided by nurse care managers is for informational and educational purposes. The information is not intended to and should not be construed to be a substitute for professional medical advice, diagnosis, or treatment. You should consult and review all information regarding any medical condition or treatment with your healthcare provider.
This overview of our Population Health Management Programs and Services is provided for informational purposes only and may be subject to change at Capital Blue Cross’ discretion. All Population Health Management Programs are subject to the terms and conditions of your benefit plan. The information provided is not a guarantee of services or payments. The information provided in this overview is not intended to be a substitute for medical advice, diagnosis, or treatment. By providing this information, Capital Blue Cross is not recommending any particular treatments or health care services.