Cost control
Strategically managing costs for our members
Drug formulary management
Through carve-in, formulary strategies are developed to achieve the overall best clinical results. We use the expertise of local practicing physicians and pharmacists, who serve on our Pharmacy and Therapeutics Committee, to ensure the formulary responds to the needs of our providers and members.
The Theon® platform uses advanced data and analytics to incorporate both medical and drug information, allowing us to better forecast the impact of newly released or soon-to-be released drugs.
Cost control for mutual customers
Plans may include prior authorization or enhanced prior authorization for certain prescription drugs, which means members may be asked to try another proven, cost-effective drug first. Many brand drugs have less expensive generic or brand alternatives that might be an option. Drugs requiring prior authorization or enhanced prior authorization are noted in members’ formularies.
Plans also includes quantity limits for certain prescription drugs to support safety.
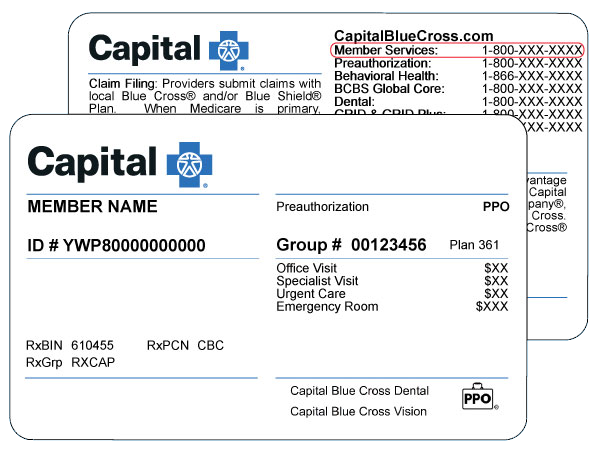
Prescription drugs that require quantity level limits are marked accordingly on the formulary. If a member’s prescription is written for more than the allowed quantity, their pharmacy will only fill up to the allowed amount. Their doctor can request an exception to quantity limits by calling the number on their Capital Blue Cross member ID card.
Plans may include a mandatory or restrictive generic substitution program to help control drug costs. Under the mandatory program, the pharmacy may replace a brand-name drug with a generic one. If a member requests the brand-name one, they will be charged the brand-name cost share plus the cost difference between the generic and brand-name medication. Under the restrictive program, their doctor can write "brand medically necessary" on the prescription.
Walgreens Specialty Pharmacy serves as our specialty drug pharmacy. If a member needs a specialty drug to manage their health condition, a patient care coordinator from Walgreens Specialty Pharmacy will work with a team of pharmacists, nurses, their doctor, and Capital Blue Cross to give personalized care that helps best manage the member’s needs.
Services include:
- Help getting prior authorization and refills
- The convenience of having drugs delivered directly to the home at no additional cost
- Free supplies, such as needles, syringes, and disposal containers
- Training and educational resources to help ensure members know how to take their medication
- Care management programs that can help members get the best results from our prescribed drug therapy
90DayMyWay® from Walgreens Specialty Pharmacy
If a plan includes this program, members must get maintenance drugs in 90-day supplies, either through home delivery or by picking them up at pharmacies that are part of the Extended Supply Network.
Want to know what pharmacy coverage could look like for your clients?
Contact your Capital Blue Cross sales representative.